Atrial Fibrillation
Atrial Fibrillation affects six million people in Europe, making it the most common Heart Rhythm disturbance (Arrhythmia). To read about how a healthy heart functions, read our article „The Healthy Heart.“
What actually happens in Atrial Fibrillation?
How is Atrial Fibrillation classified?
What are some causes and risk factors for Atrial Fibrillation?
Which symptoms characterize Atrial Fibrillation?
How is Atrial Fibrillation diagnosed?
Which treatments are recommended for Atrial Fibrillation?
What actually happens in Atrial Fibrillation?
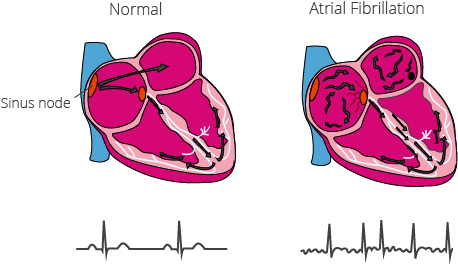
With a heart rhythm disturbance, such as Atrial Fibrillation, the natural rhythm of the heart is disrupted. Electrical impulses, originating from the Sinus Node in the Right Atrium, are responsible for maintaining a continuous, regular rhythm. With Atrial Fibrillation, the electrical impulses do not originate in the Sinus Node, but in other areas of the Atrium or in the area surrounding the pulmonary veins. The electrical impulses, with their size, form and frequency varying, are then transmitted rapidly and uncontrolled. The Atria appear to twitch, ie to „fibrillate,“ with not every impulse from the Atria being transmitted to the Ventricles. The normal contraction of the Ventricle is disrupted, causing an irregular pulse. Through poor contraction, blood stays behind and can easily clot. When a clot forms, it can travel to other organs and cause a stroke in the brain, or an embolus in the lungs.
How is Atrial Fibrillation classified?
Atrial Fibrillation is classified by the frequency and length of occurrences:
- First Diagnosed (never before diagnosed, irrespective of duration)
- Paroxysmal (sudden, self-terminating episodes lasting fewer than 7 days)
- Persistent (episodes lasting longer than 7 days that do not self-subside)
- Long-standing Persistent (lasting > 1 year, receiving treatment for rhythm control)
- Permanent (Atrial Fibrillation that is persistent, not receiving treatment)
What are some causes and risk factors for Atrial Fibrillation?
Atrial Fibrillation often emerges with increasing age. One reason for this, is the change in heart tissue, which is scarred over time. This causes the electrical signals from the atria to be improperly transmitted, disrupting the normal activity of the heart.
Additional causes of Atrial Fibrillation include:
- Valvular Heart Disease (especially a defect of the Mitral valve)
- Coronary Heart Disease
- Hyperthyroidism
- Electrolyte disturbances
- Cardiomyopathy
- Sick Sinus Syndrome
- Preexisting Atrial Flutter
In approximately half of Atrial Fibrillation cases the cause is unknown.
Many chronic diseases also increase the risk of developing Atrial Fibrillation, such as: high blood pressure, heart disease, diabetes mellitus, thyroid and lung diseases, sleep apnea or kidney disease.
Which symptoms characterize Atrial Fibrillation?
Many people affected by Atrial Fibrillation, particularly when paroxysmal in nature, often times sense nothing, or at most a light decrease in attentiveness. The most common symptoms include a racing heart, dizziness, perspiration, difficulty breathing, chest pain or anxiety.
The severity of symptoms is dependent upon how fast the heart is beating. If the heart is beating at a normal rate, only fatigue or dizziness may be perceived. If the heart is beating too quickly, one can experience the sensation of a racing heart, chest pain or difficulty breathing.
When Atrial Fibrillation is present for a longer period of time, the body becomes accustomed to its presence, and those affected may no longer experience symptoms.
How is Atrial Fibrillation diagnosed?
The diagnosis of Atrial Fibrillation can be difficult, especially when dealing with Paroxysmal Atrial Fibrillation. The workup includes an Electrocardiogram (ECG) recording, which records the electrical activity of the heart. To obtain a more comprehensive result, it is oftentimes necessary to use a long-term ECG or an Event-Recorder over the period of days. By the time one visits a Cardiologist and has an ECG performed, too much time has often passed in order to detect an abnormality. When this is the case, the patient is then sent home without a conclusive diagnosis.
Which treatments are recommended for Atrial Fibrillation?
If Atrial Fibrillation is triggered by another disorder, the initiating disorder should be treated first. In these cases Atrial Fibrillation may improve on its own.
With intermittent episode, medications are prescribed that can help bring the heart back to its normal rhythm. While these medications are very effective, they often are associated with considerable side effects, such as dizziness, fatigue or depression. Through cardioversion, the heart rhythm can be normalized via external electrical currents. Ablation (radiofrequency or cryotherapy) is an alternative surgical method of returning the heart back to its normal rhythm.
Leading a healthy lifestyle can help decrease the risk of Atrial Fibrillation.
In order to give you certainty of your heart when living with Atrial Fibrillation, we have developed CardioSecur ACTIVE. CardioSecur ACTIVE makes it possible to check your heart health any time, and anywhere, and gives you the option to share the results with your physician when necessary. CardioSecur detects Atrial Fibrillation and helps you know what to do, walking you through the next steps.