How Coronavirus Covid-19 affects the Heart
Initially, Covid-19 was mainly regarded as a disease of the respiratory tract, but there is increasing evidence that the novel coronavirus can also cause severe damage to the heart and circulation. Increased reluctance among the population to visit a doctor further increases the risk of severe outcomes.
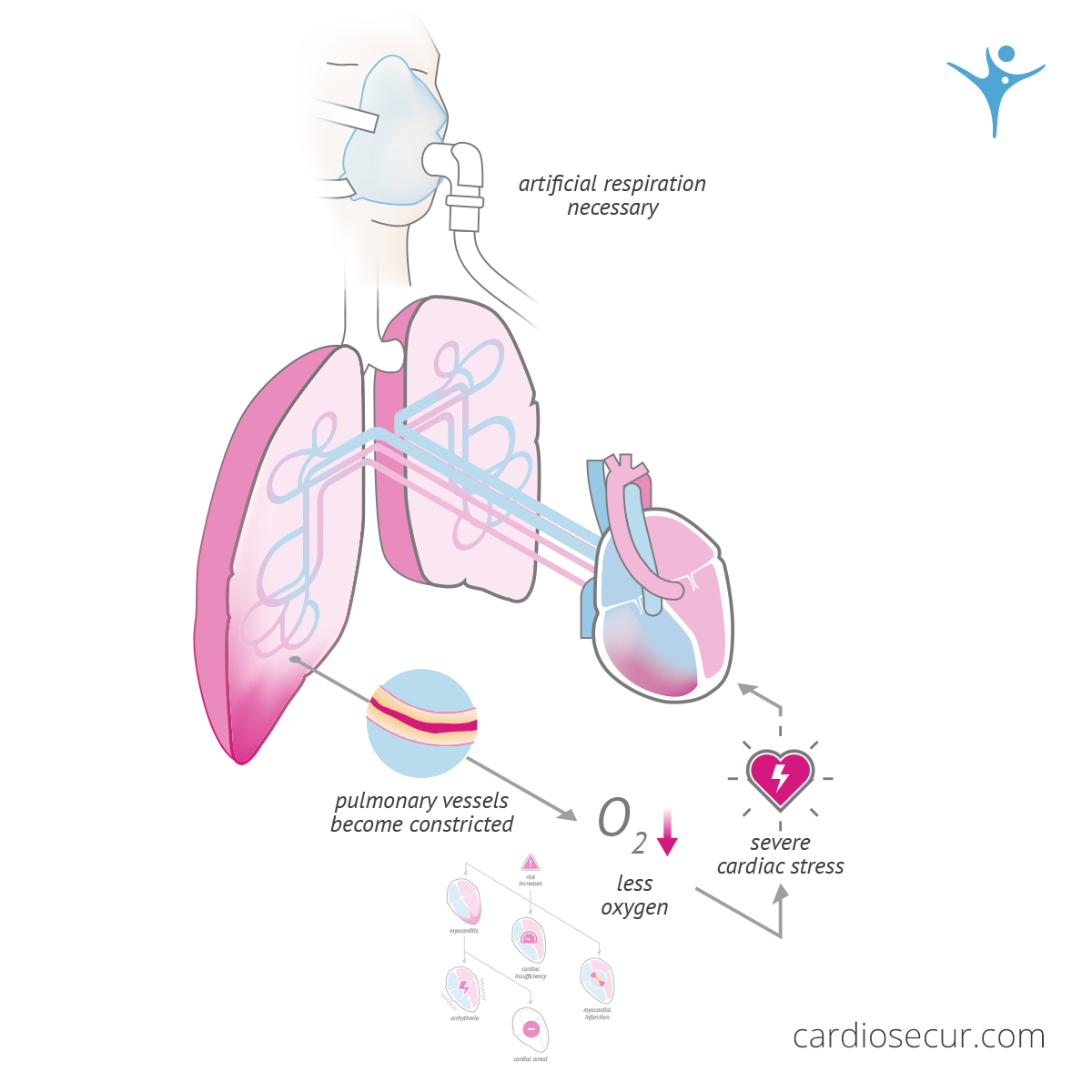
Maximum stress for the heart
Covid-19 can lead to pneumonia and this in a particularly pronounced form, because often both sides of the lungs are filled with fluid. As a result, the pulmonary vessels constrict. As a result, the body is supplied with less oxygen and the right half of the heart, which pumps blood through the lungs, is more heavily burdened. In addition, pneumonia caused by Covid-19 can last for several weeks.
If the course of the disease requires artificial respiration, this means maximum stress for the heart - especially for the right half of the heart, as increased pressure and resistance in the small circulation (pulmonary circulation) occurs. This poses a particular challenge to the cardiovascular system and thus increases the risk of a heart attack or heart failure.
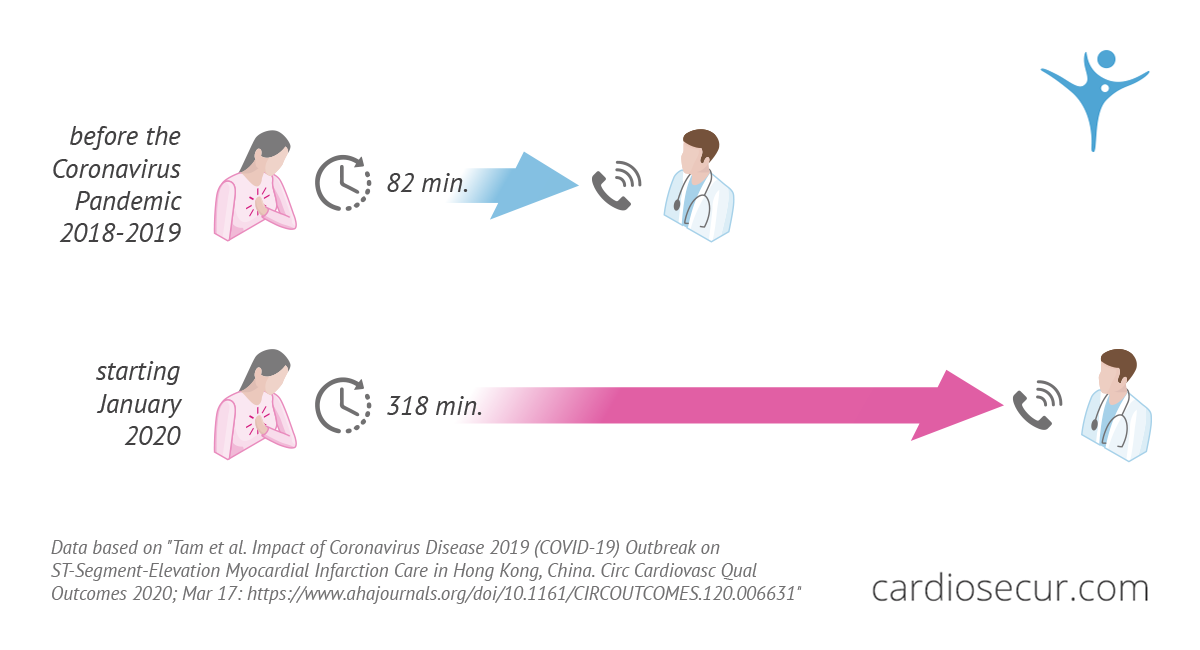
Patients avoid visits to the doctor even in cases of heart attacks
Covid-19 indirectly provokes patients to avoid doctor's visits and emergency rooms - even in the case of serious events such as heart attacks or strokes - in order to avoid a possible infection. This effect is more pronounced in heart patients, since it is now known that a severe course of COVID-19 is likely to occur in these patients in particular. The President of the German Society for General and Family Medicine (DEGAM), Prof. Dr. med. Martin Scherer, warns in an interview with the German Ärztezeitung1 that the care of cardiovascular patients could deteriorate. With reference to China and a study published there, he states that the treatment of ST elevation infarcts suffers, although these are visible in the ECG. Prior to the coronavirus pandemic (2018 - 2019), the time between the first symptoms of an ST elevation heart attack and the first contact with a physician was 82 minutes on average. From January 2020, this time increased to 318 minutes in China - an almost fourfold increase in the time it takes for patients to receive care. This is a worrying development for a disease where every minute counts (see Golden Hour).
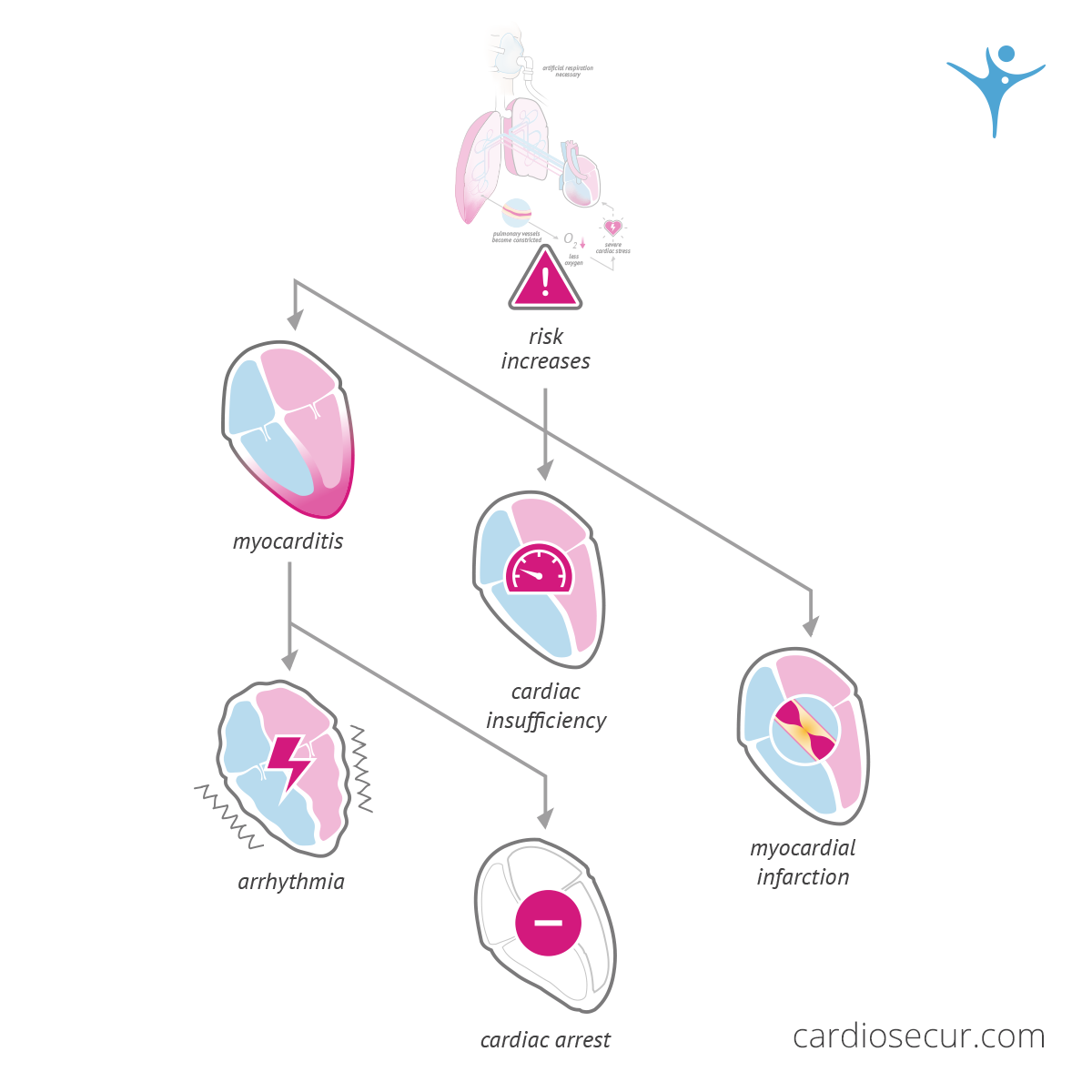
Myocarditis caused by Covid-19
For a long time, it was assumed that Covid-19 was solely a lung disease that causes pneumonia. However, when examining tissue samples at the University Hospital of Zurich, pathologists noticed that the patients also suffered from endothelial inflammation affecting various organs. The endothelium is a cell layer that forms a kind of protective shield in the vessels and regulates various processes in the microvessels. If these processes are disturbed, this can lead to circulatory disorders in the organs or body tissue, which can lead to cell death and thus to the death of the organs or tissue.
The researchers concluded that the virus not only causes pneumonia, but also directly causes systematic endotheliitis, an inflammation of the entire endothelium in the body, which affects all vascular beds - including the heart vessels. This has fatal consequences, as it causes severe microcirculatory disorders that can damage the heart and, through multiple organ failure, can lead to death.
Several case reports show that the course of these systematic endotheliits can also lead to myocarditis. Affected patients often feel weak and short of breath or even feel severe chest pain or even heart stumbling. Myocarditis can lead to cardiac arrhythmia or cardiac arrest.
Blood pressure regulation dysfunction
When attacking the body, the Covid-19 viruses dock to the most important regulatory system of blood pressure: the ACE2 receptors. Actually, ACE2 receptors ensure that substances are broken down and blood vessels are narrowed in order to increase blood pressure. If a virus docks on, the cell loses the receptor and the regulatory function is lost.
However, the topic is under discussion for another reason: In Germany, around 16 million people take so-called ACE inhibitors every day to lower their blood pressure in order to intervene in precisely this system. Therefore, both beneficial and adverse consequences are conceivable. Theoretically, ACE inhibitors could, through binding to ACE2 receptors, make it more difficult for the viruses to enter the cells and thus attenuate the disease. However, it is also possible that the intake of drugs might lead to an increase in the number of ACE2 receptors on the cell surface. At present, the influence of ACE inhibitors on the course of Covid-19 is still completely unclear. However, cardiological societies all over the world agree that patients should never stop taking their medication.
Blood coagulation disorder
Laboratory values of patients with severe Covid-19 disease indicate that blood clotting occurs significantly faster than would normally be the case. While blood clotting is normally responsible for quickly sealing injured vessels, in Covid-19 patients it can cause important blood vessels to become blocked - for example in the lungs. For example, deep vein thrombosis or pulmonary embolism has been observed in one third of Covid-19 patients requiring intensive care.
1 Ärztezeitung "Gibt es wegen SARS-CoV-2 mehr tödliche Herzinfarkte?"