What is coronary heart disease?
Coronary artery disease (CAD) is a chronic heart disease caused by narrowed coronary arteries. A total of three coronary arteries supply the heart with oxygen. A narrowing or even a blockage of one or more vessels inhibits the oxygen supply to the affected parts of the heart. This oxygen deficiency is also called myocardial ischaemia. The most common symptom of CHD is angina pectoris (AP) attacks, i.e. a feeling of stabbing, pain and tightness in the chest. However, it is not uncommon for the symptoms to radiate to other areas e.g. the back, jaw or upper abdomen . CHD favours the development of other heart diseases such as cardiac nsufficiency or cardiac arrhythmias. Acute forms of CHD are grouped together under the term acute coronary syndrome (ACS) . This includes unstable angina pectoris (IAP), i.e. sudden, severe heart complaints, heart attacks and sudden cardiac death. CHD is the most common cause of death both in Germany and worldwide.
Development of coronary heart disease
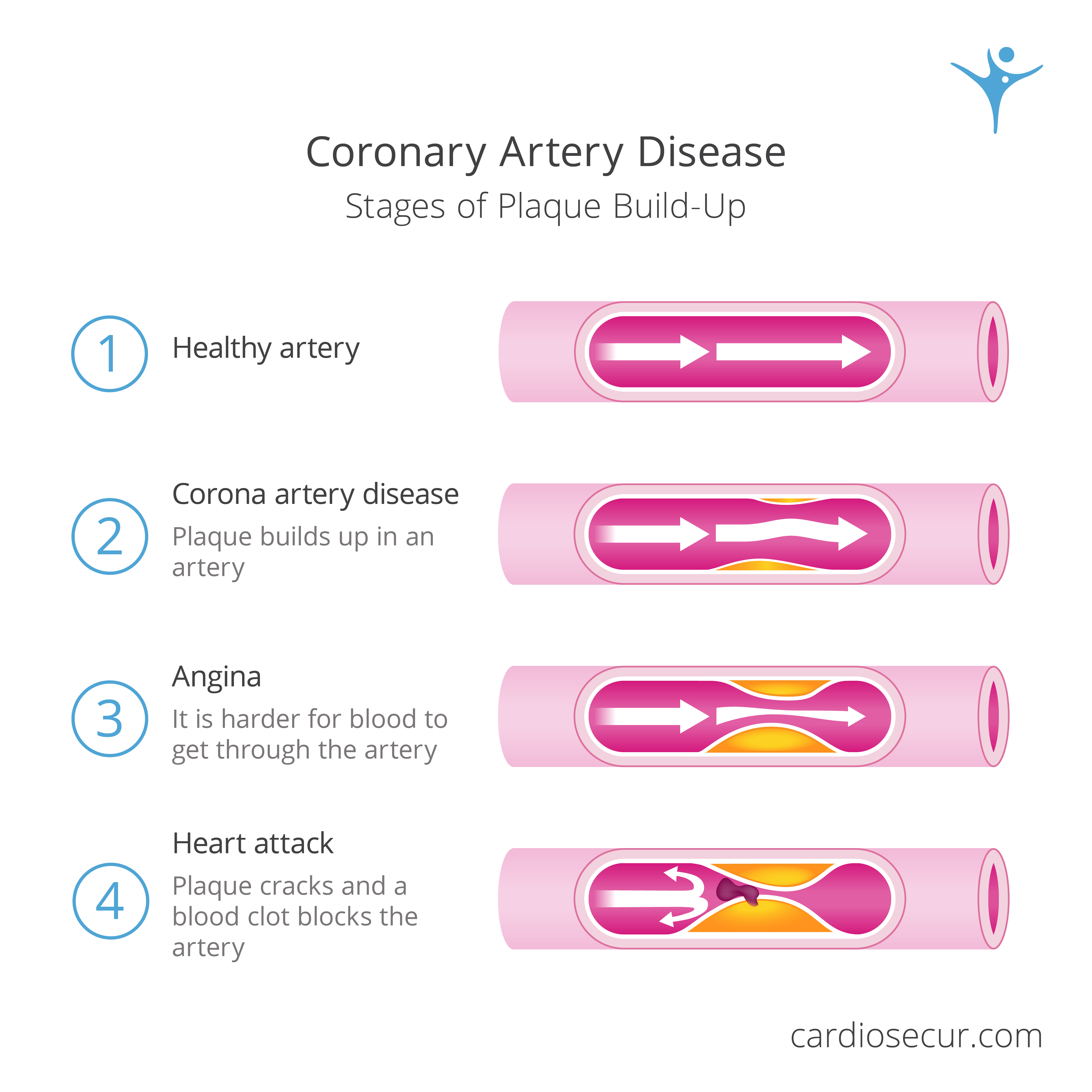
CHD develops when fats in the bloodstream, especially LDL cholesterol, are deposited in the vessel walls of the coronary arteries. The body can react to this with an inflammatory process, the concrete physiological mechanism of action of which is not entirely clear. The development of deposits is called arteriosclerosis. Growths form on the walls of the blood vessels, so-called plaques. These lead to the affected vessels thickening, narrowing and hardening. This process is often referred to as arteriosclerosis. As a result, the diameter of the vessels decreases and the blood flow is inhibited.
The tissue of the coronary vessels loses its natural elasticity and resistance due to arteriosclerosis. The resulting plaques can become inflamed and rupture. In order to close such a tear (rupture), blood corpuscles collect which can clog the vessel due to the reduced circumference and thus close it. The blood flow and the associated oxygen supply to the affected heart muscle tissue is interrupted and the tissue, which is no longer supplied with blood, dies. This process is called a heart attack. The vascular occlusion must then be invasively removed or bridged as quickly as possible.
Coronary heart disease is usually caused by a combination of factors. The risk of developing the disease can be hereditary or increased by certain pre-existing conditions. The risk is higher for men than for women. Overall, disease becomes more likely with increasing age, although the first vascular deposits can occur at a young age.
Physiological pre-existing conditions that favour the development of CHD include dyslipidemia, hypertension and diabetes mellitus.
A too high level of LDL cholesterol in the blood promotes the deposition of plaques, these fat-protein compounds on the walls of the blood vessels. Such a lipometabolic disorder (colloquially called simply cholesterol) can be hereditary or triggered by damaged organs, long-term medication, stress hormones or a diet too rich in cholesterol.
High blood pressure (hypertension), diabetes mellitus and smoking damage the inner walls of the blood vessels. These damaged vessel walls can store more fats, which in turn promotes the formation of plaques and leads to coronary heart disease.
Diagnostic procedures
Coronary heart disease is usually only discovered when it is already symptomatic, i.e. when the typical angina pectoris symptoms appear. However, CHD can also have non-specific symptoms. For example, women complain more often of abdominal pain, older people of general malaise. CHD can even be asymptomatic.
A medical history discussion can lead to an initial tentative diagnosis in the case of angina pectoris symptoms. The first step is to clarify the pain attacks with regard to the triggering circumstances, their severity and duration. Existing personal risk factors are discussed. In addition, the patient's own and the family's medical history is included in the diagnosis.
During the detailed medical examination of the body, the main focus is on looking for signs of typical pre-existing and concomitant diseases such as heart failure, arteriosclerosis in other parts of the body or diabetes mellitus.
A laboratory examination can provide further information about concomitant diseases such as diabetes mellitus and lipometabolic disorders. If a heart attack is suspected, measuring the concentration of the enzyme troponin is an indicator of acute ischaemia.
In addition to the interview, examination and laboratory diagnostics, there are other invasive and non-invasive procedures:
A resting ECG at the moment of pain is very likely to show ECG changes. Especially if the recording also looks at the right heart and the posterior wall according to the guidelines. Typical signs of infarction or cardiac arrhythmias may appear.
A resting ECG without pain sensation does not tend to show any changes or show signs of a heart attack that has already occurred but may have gone undetected as well as cardiac arrhythmias. The latter can also indicate CHD.
Other possible examinations for diagnosing CHD take place under physical stress. Usually this stress is produced by cycling (bicycle ergometry). The stress ECG measures the patient's heart flow curve under physical stress. Possible changes in the ECG curve and cardiac arrhythmias, which can indicate myocardial ischaemia, may thus become visible.
A myocardial scintigraphy also takes place under stress. The doctor injects a radioactive contrast medium (thallium) intravenously. This only accumulates in healthy areas of the heart muscle. By taking pictures with the help of a gamma camera shortly and a few hours after the injection, regions that could not absorb thallium become visible.
A stress echocardiography involves an ultrasound examination under stress. During such an examination, disturbances in the movements of the heart muscle can be observed. The so-called wall motion disturbances are caused by stenoses (narrowing of the vessels) and thus indicate CHD.
A magnetic resonance imaging (MRI) of the heart also looks for wall motion abnormalities. Such an MRI is also performed under drug-induced stress.
In invasive coronary angiography, the cardiologist injects a contrast medium into the coronary arteries with the help of a heart catheter. This allows him to recognise possible stenoses in X-ray images.
Therapeutic agents
The course of coronary heart disease can be delayed. Both medication and a change in lifestyle contribute to this.
Drug therapy mainly includes nitrates and beta-blockers. Nitrates reduce the oxygen demand of the heart and can thus be used to treat the symptoms associated with CHD. Beta-blockers reduce the heart rate and oxygen demand of the heart and thus not only relieve the symptoms of CHD, but also reduce the risk of AKS.
CHD is not curable. Stenoses that have developed cannot yet be reduced. Depending on the degree of arteriosclerosis, revascularisation of the vessels may be necessary to improve blood flow.
To stabilise and open the vessels, a so-called stent can be implanted with the help of a heart catheter. A stent is a small tube made of metal mesh that acts as a prosthesis to widen and support the affected artery from the inside.
Another method of invasive therapy is bypass surgery. Veins and arteries taken from the patient's own body (autogenous transplantation) bridge the stenosed arterial site. Bypass surgery is performed on the open heart.
Prevention and improvement of prognosis
A healthy diet, especially one low in fat - e.g. along the lines of the so-called Mediterranean diet, a balanced lifestyle with sufficient exercise, stopping smoking, reducing stress and losing weight if you are overweight can improve the prognosis of existing CHD. These measures also serve to prevent the development of coronary heart disease. In addition, pre-existing conditions should be recognised and treated.
Back