Sleep Apnea
When suffering from sleep apnea, individuals experience interruptions of breathing during sleep. Depending upon the type of sleep apnea, these pauses can last between ten seconds and two minutes, and occur more than five times per night. This causes the cardiovascular system to not receive enough oxygen, thereby greatly increasing the risk of cardiovascular diseases such as high blood pressure, stroke and heart attack. However, most people are unaware of the dangers associated with sleep apnea.
What are the different forms of sleep apnea?
What are some characteristics of obstructive sleep apnea (OSA)?
What causes obstructive sleep apnea?
What are some symptoms of obstructive sleep apnea?
How is obstructive sleep apnea treated?
What are the characteristics of central sleep apnea?
What is the correlation between sleep apnea and cardiovascular disease?
What are the different forms of sleep apnea?
Sleep apnea is divided into obstructive and central sleep apnea.
Obstructive Sleep Apnea
What are some characteristics of obstructive sleep apnea (OSA)?
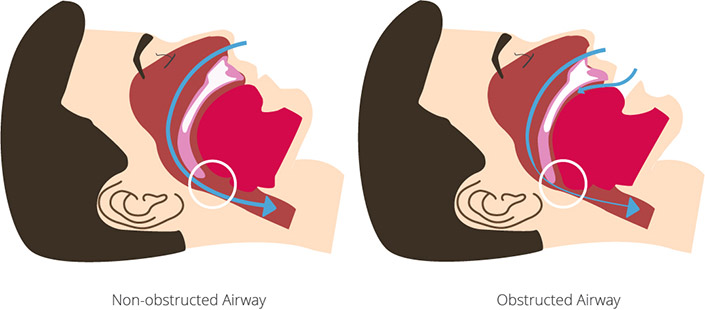
With obstructive sleep apnea (OSA), the muscles of the soft palate relax during sleep. This causes the airway to close and prevents normal breathing. The body is placed under stress as it does not receive enough oxygen, causing the blood pressure to rise, and the heart to work harder. The brain senses the disruption of breathing and the body responds with an awakening reaction (arousal). The breathing abruptly restarts, and the pulse rises. The individual briefly wakes, disrupting the normal healthy sleep cycle. The sleep disturbance, however, often goes unrecognized. If obstructive sleep apnea is untreated, the blood pressure rises leading to an increased risk of atherosclerosis and cardiovascular disease. This can further lead to heart attack, arrhythmia, stroke, or heart failure. Obstructive sleep apnea is very common: between two and four percent of adults suffer from this disorder. 15-19% of elderly men and 9-15% of elderly women are affected.
Visit our specialty articles to learn more about how high blood pressure and atherosclerosis develop and their possible side effects.
What causes obstructive sleep apnea?
Obstructive sleep apnea is caused by an instability of the upper airway. This may occur for a variety of reasons, some of which include: age, weight, gender, lifestyle, genetic factors, ethnic background, changes of the sleep-wake-cycle and the respiratory system, as well as anatomic peculiarities of the neck/pharynx (including the lower jaw). The latter leads to a receding lower jaw and tongue, which especially when in the supine position, sit too far posteriorly and can block the airway. Most affected individuals are overweight and have either a receding, small or double chin.
Additional risk factors for sleep apnea include:
- Being overweight
- Increased alcohol consumption
- Increased nicotine consumption
- Sleep or sedating medications
- Heart failure
- Malformation/malposition of the lower jaw
- Restricted breathing due to polyps
- Deviated nasal septum
- Enlarged tonsils
- Large tongue
What are some symptoms of obstructive sleep apnea?
The main symptoms of OSA include excessive daytime sleepiness with disruption of concentration and a decrease in daily performance, frequent periods of dozing off and loud/irregular snoring.
Additional symptoms of obstructive sleep apnea include:
- Interruptions of breathing lasting between 10 seconds and one minute, which are often unnoticed
- Loud, irregular snoring
- Fatigue
- Sluggishness
- Nodding off
- Interrupted sleep
- Jerking awake with the feeling of gasping for air
- Morning headaches
- Forgetfulness
- Voice changes
- Depression
How is obstructive sleep apnea treated?
CPAP therapy (continuous positive airway pressure) is one of the most common treatments for obstructive sleep apnea. With CPAP, a machine with a breathing mask supports breathing by generating a slightly elevated pressure in the airway, preventing the airway from collapsing. Another option is an adjustable oral appliance which can be used to help in anatomically keeping the airway open. A change in lifestyle (reduction in weight, stopping smoking, decreasing alcohol consumption) and avoiding sleeping on one’s back can also be beneficial. The most extreme measure is surgical intervention.
Central Sleep Apnea
What are the characteristics of central sleep apnea?
With central sleep apnea, breathing stops due to a disturbance of the central nervous system. Those suffering from cardiac insufficiency, or heart failure, often experience central sleep apnea.
A special form of central sleep apnea is Cheyne-Stokes respiration, named after the physicians John Cheyne and William Stoke. This form occurs particularly often in combination with heart failure, and is due to sensitivity of the respiratory center. It is characterized by a gradual increase and decrease in breathing effort/flow (crescendo-decrescendo pattern), occurring multiple times per minute. The breathing becomes increasingly shallower until the breathing stops (apnea). This leads to an exaggerated restart of breathing, the breaths become deeper and more exhausting, and the respiratory rate can change. In comparison to a healthy individual in which a breathing disturbance during sleep spontaneously ends, those with Cheyne-Stokes breathing experience awake, leading to sleep fragmentation.
Cheyne-Stokes respiration is often caused by insufficient circulation to the brain, such as following a stroke, damage to the central nervous system or atherosclerosis. This causes a regulatory disturbance of the brain’s respiratory center. This can be diagnosed via a polysomnography examination (ambulatory sleep test) in a sleep lab. Underlying diseases (i.e. heart failure, Diabetes mellitus, kidney disease) should be treated. Successful treatment has a positive effect on life expectancy.
Symptoms are not always present with Cheyne-Stokes breathing. Those affected do not necessarily snore more/louder than those without this disorder. However, decrease in performance, daytime sleepiness or waking up gasping for air can indicate its presence.
What is the correlation between sleep apnea and cardiovascular disease?
Sleep apnea causes high blood pressure, which is one of the main risk factors for cardiovascular disease. In this situation, high blood pressure can be difficult to treat and may also lead to an increased risk of insulin resistance (with may further progress to diabetes mellitus, another risk factor for heart disease). Additionally, heart rhythm disorders, heart attack, and sudden cardiac death can all result from high blood pressure.
With obstructive sleep apnea, the risk of heart attack is three times higher and the risk of stroke is four times higher. Additionally, those with untreated obstructive sleep apnea have a life expectancy that is decreased by approximately 10 years, and die, on average, nine years after diagnosis due to cardiovascular disease.
Pre-existing heart failure can be worsened by sleep apnea. 25-40% of those with heart failure exhibit typical the Cheyne-Stokes breathing pattern, which further accelerates heart failure. Heart failure worsens sleep apnea and vice versa. 10 percent of stroke patients with suffer from Cheyne-Stokes breathing. The consequences of heart failure paired with sleep apnea are a decreased quality of life and a shorter life expectancy, in comparison to those who suffer from heart failure only. For this reason, it is important to treat sleep apnea quickly.